An information guide on Chest Pain Causes in Africa. Introduction to Chest Pain Causes
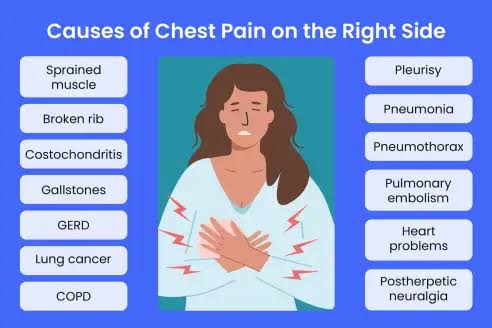
Chest pain is a common symptom that can arise from various underlying conditions affecting the heart, lungs, esophagus, or surrounding structures in the chest area1. It is crucial to understand the possible causes of chest pain, as they range from benign issues like acid reflux or gastroesophageal reflux disease (GERD) to life-threatening emergencies such as a heart attack or pulmonary embolism.
Some of the most common causes of chest pain include coronary artery disease, which occurs when a blood clot or plaque buildup obstructs blood flow to the heart muscle, leading to myocardial infarction (heart attack). Other heart problems, such as aortic dissection, aortic aneurysm, mitral valve prolapse, or heart rhythm problems, can also lead to sharp pain or discomfort in the chest.
Non-cardiac causes include lung conditions like pulmonary embolism, where a blood clot blocks the lung arteries, or inflammation of the surrounding tissues. Gastrointestinal issues, such as esophageal hypersensitivity or GERD, may mimic heart-related pain by causing acid reflux and irritation in the chest area. Rare conditions like inflammation of the heart’s lining (pericarditis) or esophagus-related disorders can also contribute to the discomfort.
Additional factors such as high blood pressure, coronary artery disease, and even structural abnormalities in the heart or vessels require prompt attention. For many people, distinguishing between a heart problem and other causes can be challenging, making it essential to seek medical help to rule out life-threatening conditions.
Common Causes of Chest Pain in Africa: From Heart Conditions to Infections
Chest pain is a concerning symptom that can arise from a variety of conditions. In Africa, its causes range from cardiovascular diseases to infectious and non-cardiac conditions. Understanding the regional prevalence and unique challenges associated with chest pain is essential for effective diagnosis and management. This guide explores the common causes of chest pain in Africa, emphasizing heart conditions, infections, and other contributing factors.
Cardiovascular Causes of Chest Pain
a. Ischemic Heart Disease (IHD)
Increasingly common in urban areas due to lifestyle changes, IHD, including angina and heart attacks, is a leading cause of chest pain.
Risk factors: Hypertension, diabetes, smoking, and high cholesterol.
Symptoms: Crushing or squeezing chest pain, often radiating to the arm or jaw.
b. Hypertension and Hypertensive Heart Disease
High blood pressure can lead to left ventricular hypertrophy and heart failure, causing chest pain.
Prevalence is high due to genetic predisposition and limited access to healthcare.
c. Pericarditis and Myocarditis
Inflammatory conditions of the heart lining (pericardium) and muscle (myocardium) often linked to infections like viral or bacterial illnesses.
Symptoms: Sharp chest pain that worsens with breathing or lying down.
d. Pulmonary Embolism (PE)
Often underdiagnosed, PE occurs when a blood clot blocks a lung artery, causing acute, sharp chest pain.
Risk factors: Prolonged immobility, sickle cell disease, and deep vein thrombosis.
Respiratory Infections and Diseases
a. Tuberculosis (TB)
A leading cause of chronic chest pain in Africa, particularly in high TB-burden regions.
Symptoms: Persistent chest pain, coughing, weight loss, and night sweats.
b. Pneumonia
Chest pain from pneumonia is common, especially in areas with limited access to vaccines and antibiotics.
Symptoms: Pleuritic chest pain (sharp pain on breathing), fever, and productive cough.
c. Pleural Effusion and Empyema
Conditions involving fluid accumulation in the pleural space can result from TB, pneumonia, or trauma, causing chest discomfort.
d. Pulmonary Diseases
Chronic obstructive pulmonary disease (COPD) and asthma can cause chest tightness, often exacerbated by environmental factors like air pollution.
Gastrointestinal Causes
a. Acid Reflux and Gastroesophageal Reflux Disease (GERD)
Commonly mistaken for cardiac chest pain, GERD causes burning chest pain, especially after meals.
Triggers: Spicy or acidic foods, obesity, and alcohol consumption.
b. Peptic Ulcers
Ulcers caused by H. pylori infections or NSAID use can result in epigastric pain radiating to the chest.
c. Esophageal Spasms
Muscle contractions in the esophagus can mimic heart-related chest pain.
Musculoskeletal and Trauma-Related Causes
a. Costochondritis
Inflammation of rib cartilage is a common non-cardiac cause of chest pain, often resulting from physical strain.
Symptoms: Tenderness on pressing the chest.
b. Trauma and Rib Fractures
Road traffic accidents and occupational injuries are common causes of musculoskeletal chest pain.
c. Fibromyalgia
A condition that can cause widespread pain, including the chest, often exacerbated by stress and fatigue.
Hematological and Sickle Cell-Related Causes
a. Acute Chest Syndrome (ACS)
A severe complication of sickle cell disease, ACS presents with chest pain, fever, and respiratory distress.
Prevalence is high in regions with endemic sickle cell anemia.
Infectious Causes Beyond Respiratory Conditions
a. HIV/AIDS and Opportunistic Infections
HIV-infected individuals often experience chest pain due to conditions like TB, pneumocystis pneumonia, or Kaposi sarcoma.
b. Fungal Infections
In regions with high HIV prevalence, fungal infections like histoplasmosis can cause chronic chest pain.
Psychological Causes
a. Anxiety and Panic Disorders
Mental health issues are often overlooked but can cause chest pain through hyperventilation and stress.
b. Post-Traumatic Stress Disorder (PTSD)
Individuals in conflict-affected areas may experience chest pain linked to psychological distress.
Diagnostic Challenges and Considerations
Limited Resources: Many rural areas lack advanced diagnostic tools like ECGs or imaging for heart and lung diseases.
Overlap of Symptoms: Differentiating between cardiac, respiratory, and gastrointestinal causes can be difficult.
Delayed Care: Late presentation due to financial or logistical barriers contributes to worse outcomes.
Prevention and Management Strategies
Public Awareness: Educate communities about risk factors and early symptoms of serious chest pain causes.
Vaccination Campaigns: Widespread use of vaccines for pneumonia and influenza can reduce respiratory-related chest pain.
Improved Access to Healthcare: Strengthening primary care systems to diagnose and manage chest pain early.
Lifestyle Interventions: Promote heart-healthy diets, smoking cessation, and physical activity to reduce cardiovascular risks.
Antiretroviral Therapy (ART): For HIV patients, effective ART reduces the risk of opportunistic infections causing chest pain.
Chest pain in Africa stems from diverse causes, including heart conditions, infections like tuberculosis, gastrointestinal issues, and psychological factors. Addressing these causes requires a holistic approach combining prevention, early diagnosis, and effective treatment. With enhanced healthcare access and education, the burden of chest pain-related morbidity and mortality can be significantly reduced in African populations.
Explore cardiovascular and non-cardiovascular causes of chest pain, such as coronary artery disease, tuberculosis, and pneumonia.
The Role of Tuberculosis and Respiratory Infections in Chest Pain Across Africa
Chest pain is a significant symptom of various medical conditions, including respiratory infections and tuberculosis (TB). In Africa, where respiratory diseases remain a leading cause of morbidity and mortality, understanding their role in chest pain is crucial for effective healthcare delivery. This guide explores how TB and other respiratory infections contribute to chest pain, their prevalence, clinical presentation, challenges in diagnosis and treatment, and strategies for management.
The Burden of Respiratory Infections in Africa
Prevalence: Respiratory infections, including TB, pneumonia, and pleural diseases, are among the leading causes of hospital admissions and deaths in Africa.
High-Risk Groups: Vulnerable populations such as children under five, the elderly, individuals with HIV/AIDS, and those living in poverty are disproportionately affected.
Environmental Factors: Overcrowding, poor ventilation, and exposure to indoor air pollution from cooking fuels exacerbate the prevalence of these infections.
Tuberculosis and Its Role in Chest Pain
a. Overview of Tuberculosis (TB)
Epidemiology: Africa has one of the highest TB burdens globally, accounting for a significant proportion of new and recurrent cases.
Cause: TB is caused by Mycobacterium tuberculosis, which primarily affects the lungs but can also involve other organs.
Transmission: Spread via respiratory droplets, TB thrives in settings with high population density and poor healthcare access.
b. Chest Pain in Pulmonary TB
Pulmonary TB often presents with chest pain as a symptom, typically due to the following:
Pleural Involvement: Infection of the pleural space leads to pleuritic chest pain (sharp pain worsened by breathing or coughing).
Lung Tissue Damage: TB causes inflammation and cavitation in the lungs, contributing to discomfort and pain.
Chronic Cough: Persistent coughing strains chest muscles, leading to musculoskeletal chest pain.
c. Complications Leading to Chest Pain
Pleural Effusion: Fluid accumulation in the pleural space causes chest tightness and discomfort.
Empyema: Pus in the pleural cavity results in severe chest pain and systemic symptoms like fever.
Tuberculous Pericarditis: Involvement of the heart’s lining can cause constrictive pericarditis, leading to chest pain and difficulty breathing.
Other Respiratory Infections and Chest Pain
a. Pneumonia
Cause: Bacterial, viral, or fungal infections, often secondary to poor immune function or comorbidities like HIV.
Symptoms: Pleuritic chest pain, fever, and productive cough are hallmark signs.
Burden in Africa: Pneumonia is a leading cause of death among children under five, emphasizing the need for timely vaccination and treatment.
b. Acute Bronchitis
Often viral in origin, acute bronchitis causes inflammation of the bronchial tubes, resulting in chest discomfort and a persistent cough.
c. COVID-19
The COVID-19 pandemic highlighted the role of viral respiratory infections in causing chest pain due to lung inflammation and complications like pneumonia and pulmonary embolism.
d. Pulmonary Fungal Infections
Conditions like histoplasmosis and cryptococcosis are more common in immunocompromised individuals, particularly those with HIV/AIDS, and can mimic TB symptoms, including chest pain.
Diagnosis Challenges in Africa
a. Limited Healthcare Resources
Access to diagnostic tools like chest X-rays, CT scans, and microbiological tests is often limited in rural and underserved areas.
b. Overlapping Symptoms
Many respiratory conditions present similarly, making it difficult to distinguish TB from pneumonia, bronchitis, or other infections without advanced testing.
c. Delayed Diagnosis
Social stigma, lack of awareness, and financial barriers often delay the diagnosis of TB and respiratory infections, increasing the risk of complications.
Management of TB and Respiratory Infections
a. Tuberculosis Treatment
Standard Therapy: A six-month regimen of first-line anti-TB drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) is the standard treatment.
Drug-Resistant TB: Multidrug-resistant TB (MDR-TB) requires more extended and complex treatments, which pose significant challenges in Africa.
b. Pneumonia Management
Antibiotics: Bacterial pneumonia is treated with appropriate antibiotics, while viral infections require supportive care.
Vaccination: Pneumococcal and Haemophilus influenzae type B (Hib) vaccines are critical for prevention, especially in children.
c. Addressing Co-Infections
TB and HIV co-infection is common in Africa, necessitating integrated management strategies, including antiretroviral therapy (ART).
d. Supportive Care
Oxygen therapy, pain management, and nutritional support are vital components of care for patients with severe infections.
Prevention Strategies
a. TB Control Programs
Expanded access to diagnostic services and directly observed therapy (DOT) programs have been effective in many regions.
Community awareness campaigns help reduce stigma and promote early testing.
b. Vaccination
The BCG vaccine for TB and pneumococcal vaccines for pneumonia are critical in reducing disease burden.
c. Environmental Improvements
Reducing indoor air pollution, improving ventilation, and minimizing overcrowding are essential preventive measures.
d. Addressing Risk Factors
Strengthening health systems to manage comorbidities like HIV, diabetes, and malnutrition can reduce susceptibility to respiratory infections.
The Way Forward
a. Research and Innovation
Investment in diagnostics, such as rapid molecular tests for TB, can improve early detection and treatment outcomes.
Development of more effective vaccines for TB and respiratory infections is urgently needed.
b. Healthcare Infrastructure
Scaling up healthcare access in rural and underserved areas is essential for timely diagnosis and management.
c. Integrated Care
Programs that address TB, HIV, and other respiratory diseases together can improve efficiency and patient outcomes.
Tuberculosis and respiratory infections are significant contributors to chest pain in Africa, reflecting the continent’s dual burden of infectious and non-communicable diseases. Addressing these conditions requires a multifaceted approach that includes improving access to diagnostics, expanding vaccination coverage, and integrating care for co-infections. By tackling the underlying causes and barriers to care, Africa can reduce the impact of these diseases and improve the health and well-being of its population.
Understanding Heart Disease and Chest Pain in African Communities
Heart disease is a major cause of morbidity and mortality worldwide, including in African communities. Chest pain, one of the most common symptoms of heart disease, often signals underlying cardiovascular issues. However, the presentation, prevalence, and management of heart disease in African communities are influenced by unique social, economic, and healthcare challenges. This guide explores the connection between heart disease and chest pain in Africa, their causes, risk factors, challenges in healthcare, and strategies for prevention and management.
Overview of Heart Disease in African Communities
a. Prevalence and Burden
Cardiovascular diseases (CVDs) are the leading cause of death globally, and their prevalence is rising in Africa.
In African communities, the dual burden of communicable diseases (e.g., tuberculosis, HIV) and non-communicable diseases (e.g., hypertension, diabetes) complicates the diagnosis and management of heart disease.
Urbanization and lifestyle changes are contributing to the growing burden of heart disease.
b. Heart Disease and Chest Pain
Chest pain is a key symptom of various heart conditions, including ischemic heart disease, pericarditis, and heart failure.
It is critical to differentiate cardiac chest pain from non-cardiac causes, such as musculoskeletal, respiratory, or gastrointestinal issues, to ensure timely and accurate treatment.
Types of Heart Diseases Causing Chest Pain
a. Ischemic Heart Disease (IHD)
Cause: Narrowing of coronary arteries due to atherosclerosis, reducing blood flow to the heart.
Symptoms: Angina pectoris (chest discomfort), which may radiate to the jaw, neck, or arm.
Risk Factors: High blood pressure, smoking, diabetes, and high cholesterol.
b. Hypertensive Heart Disease
Cause: Chronic high blood pressure leading to thickening of the heart muscle.
Symptoms: Chest pain, shortness of breath, and fatigue.
Impact in Africa: Hypertension is widespread due to lifestyle factors, low awareness, and inadequate treatment.
c. Rheumatic Heart Disease (RHD)
Cause: Complications of untreated streptococcal throat infections leading to heart valve damage.
Symptoms: Chest pain, palpitations, and breathlessness.
Prevalence: High in rural African communities with limited access to healthcare.
d. Pericarditis
Cause: Inflammation of the pericardium, often due to infections (e.g., tuberculosis) or autoimmune diseases.
Symptoms: Sharp chest pain that worsens with breathing or lying flat.
e. Heart Failure
Cause: Inability of the heart to pump blood effectively, often due to ischemic heart disease or hypertension.
Symptoms: Chest pain, fluid retention, and difficulty breathing.
Risk Factors for Heart Disease in African Communities
a. Modifiable Risk Factors
- Hypertension: A leading cause of heart disease, exacerbated by high salt intake and limited access to medication.
- Diabetes: Rising rates of diabetes increase the risk of ischemic heart disease and heart failure.
- Smoking: Tobacco use is a significant contributor to coronary artery disease.
- Unhealthy Diets: Increased consumption of processed foods and reduced physical activity contribute to obesity and heart disease.
b. Non-Modifiable Risk Factors
- Genetics: Familial predisposition to hypertension and heart disease.
- Age and Gender: Older adults and men are at higher risk of ischemic heart disease, while postmenopausal women have increased risks due to hormonal changes.
c. Socioeconomic Factors
Poverty, limited healthcare access, and lack of awareness about heart disease exacerbate the problem in African communities.
Challenges in Diagnosis and Treatment
a. Delayed Diagnosis
Chest pain is often attributed to non-cardiac causes, delaying the diagnosis of heart disease.
Limited access to diagnostic tools like ECG, echocardiography, and blood tests in rural areas compounds the problem.
b. Healthcare Infrastructure
Shortages of trained cardiologists and specialized facilities restrict timely intervention for heart disease.
c. Affordability
Many African communities face financial barriers to accessing medications, such as antihypertensives, statins, and anticoagulants.
d. Co-Morbidities
The coexistence of infectious diseases like TB and HIV complicates the treatment of heart conditions.
Management Strategies for Heart Disease and Chest Pain
a. Acute Management
Patients presenting with chest pain suggestive of a heart attack require immediate medical attention, including oxygen therapy, antiplatelet drugs, and thrombolysis.
b. Long-Term Management
- Lifestyle Changes:
Promoting healthy eating, regular physical activity, and smoking cessation.
- Medication:
Use of antihypertensives, statins, and aspirin for long-term risk reduction.
- Regular Monitoring:
Blood pressure, cholesterol, and glucose level checks to prevent complications.
c. Surgical Interventions
For severe cases, procedures like coronary artery bypass grafting (CABG) or valve repair/replacement may be necessary.
Prevention Strategies
a. Community Education
Raising awareness about heart disease risk factors and early symptoms can encourage timely medical consultations.
b. Screening Programs
Implementing community-based blood pressure and cholesterol screenings to identify at-risk individuals early.
c. Policy and Advocacy
Governments must prioritize funding for non-communicable diseases, improving healthcare access and affordability.
d. Control of Infectious Diseases
Addressing rheumatic fever and TB can reduce cases of rheumatic and pericardial heart disease.
The Role of Technology and Innovation
Telemedicine: Providing rural communities with access to cardiology consultations via telehealth.
Portable Diagnostic Tools: Expanding access to mobile ECG devices and point-of-care tests.
Digital Health Campaigns: Using social media to spread awareness about heart disease prevention and management.
Heart disease is a growing public health challenge in African communities, with chest pain serving as a key indicator of underlying cardiovascular conditions. The unique interplay of risk factors, limited healthcare resources, and socio-economic barriers demands a tailored approach to prevention, diagnosis, and management. Strengthening healthcare systems, promoting awareness, and addressing modifiable risk factors are essential to reducing the burden of heart disease and improving outcomes for patients experiencing chest pain across Africa.
Musculoskeletal Chest Pain: An Overlooked Issue in Africa
Musculoskeletal chest pain, often overshadowed by more life-threatening causes of chest discomfort, is a common yet underdiagnosed condition in Africa. While cardiac and respiratory diseases dominate the discussion around chest pain, musculoskeletal causes often go unrecognized, leading to unnecessary investigations and treatments. This guide explores the prevalence, causes, diagnosis, and management of musculoskeletal chest pain in African communities, emphasizing the importance of awareness and appropriate care.
Understanding Musculoskeletal Chest Pain
Musculoskeletal chest pain refers to discomfort originating from the muscles, bones, or connective tissues of the chest wall. Unlike pain caused by cardiac or pulmonary conditions, it is typically non-life-threatening but can significantly impact quality of life.
Key Features of Musculoskeletal Chest Pain
Localized Pain: Often confined to a specific area, such as the ribs, sternum, or intercostal muscles.
Aggravated by Movement: Activities like deep breathing, twisting, or pressing the affected area usually worsen the pain.
Non-Radiating: Unlike cardiac pain, it does not radiate to distant areas like the jaw or arm.
Prolonged Discomfort: May persist for weeks or months if not addressed.
Causes of Musculoskeletal Chest Pain in Africa
a. Trauma and Physical Strain
Manual Labor: Many African communities rely on physically demanding jobs, such as farming and construction, which can strain chest wall muscles.
Injuries: Rib fractures, contusions, or sternoclavicular joint dislocations from accidents or falls are common contributors.
b. Costochondritis
Definition: Inflammation of the costochondral junctions where the ribs meet the sternum.
Symptoms: Sharp, localized pain that worsens with palpation or physical activity.
Triggers: Can result from repetitive strain, coughing, or minor chest trauma.
c. Fibromyalgia
A chronic condition causing widespread musculoskeletal pain, often including chest pain. It is underdiagnosed in African settings due to limited awareness.
d. Infections
Tuberculosis of the Rib Cage: TB can affect the chest wall bones, leading to chronic pain and swelling.
Herpes Zoster (Shingles): Painful rash and nerve irritation along the chest wall, often mistaken for cardiac pain.
e. Arthritis and Bone Disorders
Rheumatoid Arthritis: Can involve the costosternal joints, causing chest pain.
Osteoporosis: Common in postmenopausal women and malnourished individuals, it increases the risk of rib fractures.
f. Psychogenic Factors
Stress and Anxiety: Psychological distress can manifest as chest pain due to tension in the chest wall muscles.
Somatization Disorders: Physical symptoms without a medical cause are not uncommon in communities with limited mental health resources.
Challenges in Diagnosing Musculoskeletal Chest Pain
a. Misdiagnosis
Many patients with musculoskeletal chest pain undergo unnecessary cardiac or pulmonary investigations due to overlapping symptoms.
b. Limited Healthcare Resources
Access to imaging (e.g., X-rays, MRIs) and specialist consultations is often restricted in rural African settings.
c. Stigma and Lack of Awareness
Patients and healthcare providers may overlook musculoskeletal pain, attributing it to minor causes or psychological issues.
Differentiating Musculoskeletal Pain from Cardiac and Pulmonary Causes
a. Key Differentiating Factors
b. Role of History and Physical Examination
A thorough clinical history and detailed physical exam can identify tender points, inflammation, or trauma.
Diagnostic imaging is rarely needed unless there is suspicion of fractures or infections.
Management of Musculoskeletal Chest Pain
a. Non-Pharmacological Approaches
- Rest and Activity Modification: Avoiding activities that aggravate the pain.
- Physical Therapy: Strengthening and stretching exercises for the chest wall muscles.
- Heat or Ice Packs: Effective for relieving inflammation and discomfort.
b. Medications
- Pain Relievers:
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen for pain and inflammation.
Paracetamol for milder pain relief.
- Muscle Relaxants: For spasm-related chest pain.
- Corticosteroid Injections: In cases of severe costochondritis or arthritis.
c. Treating Underlying Causes
Infections: Antibiotics for bacterial infections or antiviral medications for herpes zoster.
Osteoporosis: Calcium and vitamin D supplementation alongside anti-osteoporotic drugs.
Psychological Support: Counseling or therapy for stress-induced pain.
Preventing Musculoskeletal Chest Pain
a. Workplace Ergonomics
Providing education and tools to reduce strain during manual labor.
b. Early Management of Trauma
Immediate care for injuries to prevent chronic pain syndromes.
c. Public Awareness
Educating communities about the non-threatening nature of musculoskeletal chest pain and the importance of seeking appropriate care.
Addressing Healthcare Barriers in Africa
a. Training for Healthcare Providers
Increasing awareness among clinicians to recognize and appropriately treat musculoskeletal chest pain.
b. Community Health Programs
Utilizing community health workers to provide basic care and education in rural areas.
c. Affordable Treatment Options
Ensuring that pain-relief medications and physical therapy resources are accessible to low-income populations.
Musculoskeletal chest pain, while often non-life-threatening, is a significant cause of discomfort and disability in African communities. Misdiagnosis and underdiagnosis of this condition can lead to unnecessary treatments and prolonged suffering. By improving awareness, training healthcare providers, and addressing healthcare disparities, musculoskeletal chest pain can be effectively managed and its impact minimized. Recognizing this overlooked issue is crucial to improving the quality of life for affected individuals and ensuring a more holistic approach to healthcare in Africa.
Chest Pain in Rural Africa: Challenges in Diagnosis and Treatment
Chest pain is a common medical symptom that often signals underlying health issues ranging from benign conditions to life-threatening diseases. In rural Africa, chest pain poses unique challenges due to limited healthcare infrastructure, socio-economic factors, and the coexistence of infectious and non-communicable diseases. This guide explores the causes, diagnostic challenges, and treatment hurdles for chest pain in rural African settings, offering insights into strategies for improvement.
Understanding Chest Pain in Rural Africa
Chest pain can originate from various systems, including the cardiovascular, respiratory, musculoskeletal, gastrointestinal, and psychological systems. In rural Africa, the causes of chest pain often reflect the epidemiology of diseases prevalent in these areas.
a. Prevalence and Burden
Chest pain is a frequent reason for seeking healthcare, but the burden is poorly quantified due to limited data collection and reporting in rural settings.
Late presentation and misdiagnosis can lead to high morbidity and mortality.
b. Importance of Early Diagnosis
Early diagnosis is critical to managing life-threatening conditions such as acute coronary syndromes, pulmonary embolism, or tuberculosis.
Delays in diagnosis often result from poor access to healthcare and lack of awareness among patients and healthcare providers.
Common Causes of Chest Pain in Rural Africa
a. Cardiovascular Causes
- Ischemic Heart Disease (IHD)
Rare but increasing due to urbanization and lifestyle changes.
Often underdiagnosed due to limited access to diagnostic tools like ECGs and blood markers.
- Hypertension and Hypertensive Heart Disease
Widespread in rural communities, with complications like heart failure presenting as chest pain.
- Pericarditis and Rheumatic Heart Disease
Frequently associated with infections, including tuberculosis and streptococcal infections.
- Aortic Dissection
Rare but catastrophic, often missed due to lack of imaging facilities.
b. Respiratory Causes
- Tuberculosis (TB)
A major cause of chest pain, particularly pleuritic pain due to pleural involvement.
High prevalence in sub-Saharan Africa exacerbates the burden.
- Pneumonia and Pulmonary Infections
Common in areas with limited access to vaccines and antibiotics.
Often associated with HIV, which is prevalent in many rural African regions.
- Pulmonary Embolism (PE)
Underdiagnosed due to lack of diagnostic imaging and awareness.
c. Musculoskeletal Causes
Conditions like costochondritis, rib fractures, and muscle strain are common due to physical labor.
Often misinterpreted as cardiac pain, leading to unnecessary interventions.
d. Gastrointestinal Causes
Acid reflux disease and peptic ulcers often mimic cardiac chest pain, causing diagnostic confusion.
e. Psychosomatic and Anxiety-Related Causes
Psychological factors, exacerbated by socio-economic stressors, often manifest as chest pain in rural populations.
Challenges in Diagnosis
a. Limited Healthcare Infrastructure
Diagnostic Tools: Lack of ECG machines, X-ray facilities, and laboratory tests limits the ability to identify causes of chest pain.
Specialist Access: Cardiologists, pulmonologists, and other specialists are often unavailable in rural areas.
b. Overlapping Symptoms
Coexisting infectious and non-communicable diseases blur the clinical presentation, complicating diagnosis.
c. Cultural and Socio-Economic Barriers
Traditional beliefs and stigma associated with diseases like TB or HIV delay patients from seeking care.
Poverty often prevents patients from affording transportation or treatment.
d. Limited Awareness Among Healthcare Workers
Rural health workers may lack training in differentiating between cardiac and non-cardiac chest pain.
Misdiagnosis often leads to inappropriate treatments or referrals.
Treatment Challenges
a. Access to Medications and Supplies
Essential medications like antiplatelets, antihypertensives, and antibiotics are often unavailable or unaffordable.
Stockouts of TB medications and vaccines are common in rural clinics.
b. Emergency Care Deficiencies
Absence of ambulance services and trained personnel delays treatment for acute conditions like heart attacks or pulmonary embolisms.
c. Follow-Up Care
Chronic conditions like hypertension and ischemic heart disease require long-term follow-up, which is rarely feasible in rural settings.
d. Co-Management of Infectious Diseases
Patients with HIV or TB often require coordinated care for their primary disease and related complications causing chest pain.
Overburdened rural healthcare systems struggle to provide integrated care.
Strategies for Improvement
a. Strengthening Primary Healthcare Systems
Equip rural health facilities with basic diagnostic tools like ECG machines and X-ray units.
Train healthcare workers to recognize and manage common causes of chest pain.
b. Community Education
Educate communities about the warning signs of serious conditions like heart attacks or TB.
Encourage early healthcare-seeking behavior to reduce delays in diagnosis.
c. Telemedicine and Mobile Clinics
Leverage telemedicine to connect rural clinics with specialists in urban centers.
Deploy mobile clinics to provide diagnostic services and treatment in remote areas.
d. Improving Supply Chains
Ensure consistent availability of essential medications and diagnostic supplies in rural healthcare facilities.
e. Integrating Disease Management Programs
Combine TB, HIV, and non-communicable disease management programs to improve care coordination.
f. Policy and Funding Support
Advocate for increased government and international funding to address healthcare disparities in rural areas.
Chest pain in rural Africa is a complex issue influenced by limited healthcare infrastructure, diverse disease burdens, and socio-economic barriers. Addressing the challenges in diagnosis and treatment requires a multi-faceted approach that includes strengthening primary healthcare systems, community education, and leveraging technology. By prioritizing these efforts, rural communities can achieve better outcomes for patients experiencing chest pain, ultimately improving overall health and well-being.
Gastrointestinal Causes of Chest Pain in African Populations
Chest pain is a concerning symptom often associated with cardiac or respiratory conditions. However, gastrointestinal (GI) issues are significant contributors to chest pain, especially in African populations where infections, dietary habits, and healthcare access play a crucial role. This guide explores the gastrointestinal causes of chest pain, their prevalence in Africa, diagnostic challenges, and management strategies.
Overview of Gastrointestinal Causes of Chest Pain
Gastrointestinal chest pain arises from conditions affecting the esophagus, stomach, or other parts of the digestive system. It is often mistaken for cardiac pain due to its location and overlapping symptoms. In African settings, specific GI conditions, such as infections and acid-related disorders, are prevalent and require targeted attention.
Key Characteristics of Gastrointestinal Chest Pain
Often burning or sharp, localized behind the breastbone.
May worsen after eating or lying down.
Frequently accompanied by GI symptoms such as nausea, vomiting, or bloating.
Non-radiating and usually not associated with physical exertion.
Common Gastrointestinal Causes of Chest Pain in Africa
a. Gastroesophageal Reflux Disease (GERD)
Description: Reflux of stomach acid into the esophagus causes irritation and pain.
Symptoms: Heartburn, regurgitation, and difficulty swallowing.
Prevalence: Increasing due to urbanization, dietary changes, and obesity in African populations.
b. Esophageal Spasms and Motility Disorders
Description: Abnormal contractions of the esophagus leading to pain and swallowing difficulty.
Symptoms: Sudden chest pain unrelated to eating or exercise.
Triggers: Stress, extreme temperatures in food or drinks.
c. Peptic Ulcer Disease (PUD)
Description: Ulcers in the stomach or duodenum caused by Helicobacter pylori infection or NSAID use.
Symptoms: Epigastric pain radiating to the chest, often relieved by antacids.
Prevalence: High in African populations due to poor sanitation and widespread H. pylori infection.
d. Esophagitis
Description: Inflammation of the esophagus caused by acid reflux, infections, or irritants.
Symptoms: Painful swallowing and burning chest pain.
Common in: HIV-positive individuals due to fungal or viral infections.
e. Hiatal Hernia
Description: Part of the stomach pushes into the chest cavity through the diaphragm.
Symptoms: Heartburn, regurgitation, and chest discomfort.
Risk Factors: Obesity and chronic coughing.
f. Gallbladder Disease
Description: Gallstones or inflammation of the gallbladder causing referred pain to the chest.
Symptoms: Right upper abdominal pain radiating to the chest, nausea, and fatty food intolerance.
Prevalence: Rising due to dietary changes in urbanized African areas.
g. Infectious Esophagitis
Description: Esophageal inflammation caused by fungal (e.g., Candida), viral (e.g., herpes), or bacterial infections.
At-Risk Populations: Immunocompromised individuals, including those with HIV/AIDS.
h. Functional GI Disorders
Description: Conditions like irritable bowel syndrome (IBS) that manifest with chest pain despite no structural abnormalities.
Symptoms: Often associated with stress and psychological factors.
Risk Factors in African Populations
a. Dietary Habits
High consumption of spicy, fatty, or acidic foods can exacerbate GERD and peptic ulcers.
Limited fiber intake contributes to gallbladder issues and motility disorders.
b. Infections
High prevalence of H. pylori infection due to poor water and food hygiene.
Opportunistic infections in HIV/AIDS patients, leading to esophagitis.
c. Healthcare Barriers
Limited access to diagnostic tools like endoscopy.
Over-the-counter availability of NSAIDs, leading to misuse and ulcer formation.
d. Socio-Economic Factors
Poor living conditions increase exposure to infections.
Lack of awareness leads to delayed diagnosis and treatment.
- Diagnostic Challenges
a. Overlap with Cardiac Conditions
Symptoms of GERD and esophageal spasm mimic angina, leading to misdiagnosis.
Lack of advanced diagnostic facilities complicates differentiation.
b. Limited Diagnostic Resources
Endoscopy, manometry, and imaging are often unavailable in rural and low-resource settings.
c. Cultural Beliefs
Misattribution of chest pain to spiritual or supernatural causes delays medical consultation.
d. Co-Morbid Conditions
HIV/AIDS complicates the clinical picture, especially in cases of infectious esophagitis.
Management of Gastrointestinal Chest Pain
a. General Treatment Approaches
- Lifestyle Modifications:
Avoiding trigger foods (spicy, fatty, or acidic foods).
Eating smaller meals and avoiding lying down immediately after eating.
Weight loss in obese individuals.
- Pharmacological Interventions:
Antacids and Proton Pump Inhibitors (PPIs) for GERD and esophagitis.
H. pylori Eradication Therapy for peptic ulcers.
Prokinetics for motility disorders.
Analgesics for gallbladder-related pain, avoiding NSAIDs if ulcers are present.
- Surgical Interventions:
Cholecystectomy for gallbladder disease.
Fundoplication for severe GERD with hiatal hernia.
b. Management in Low-Resource Settings
Empirical treatment for H. pylori in areas with high prevalence.
Use of symptom-based treatment algorithms when diagnostic tools are unavailable.
c. Integrating Community Health Workers
Training to identify warning signs of severe GI disorders and refer appropriately.
Educating patients on dietary and lifestyle changes.
Preventing Gastrointestinal Chest Pain
a. Improving Hygiene
Promoting access to clean water and sanitation to reduce H. pylori transmission.
b. Public Health Education
Raising awareness about the risks of NSAID overuse.
Encouraging healthy dietary practices.
c. Enhancing Healthcare Access
Expanding availability of diagnostic tools like endoscopy in rural areas.
Providing affordable medications for common GI disorders.
Gastrointestinal causes of chest pain are significant in African populations due to a combination of dietary, infectious, and socio-economic factors. While conditions like GERD, peptic ulcers, and esophagitis are common, they are often overshadowed by more urgent cardiac or respiratory conditions. Addressing these issues requires a comprehensive approach involving improved diagnostic access, community education, and integration of GI care into primary healthcare systems. By prioritizing these efforts, the burden of GI-related chest pain in African populations can be significantly reduced, improving overall health outcomes.
Psychological and Stress-Related Chest Pain in Africa
Chest pain is a widely recognized symptom often associated with physical health conditions, particularly cardiac or respiratory issues. However, psychological and stress-related factors are also significant contributors to chest pain, often underdiagnosed and poorly understood in African contexts. This guide examines the causes, prevalence, diagnostic challenges, and management strategies for psychological and stress-related chest pain in Africa.
Understanding Psychological and Stress-Related Chest Pain
Psychological and stress-related chest pain, also referred to as psychogenic chest pain or non-cardiac chest pain (NCCP), originates from emotional or mental health issues rather than physical causes.
Key Characteristics
Often described as a tightness, pressure, or aching sensation in the chest.
May occur during stressful situations or after experiencing psychological distress.
Unaccompanied by physical signs of heart disease or respiratory issues.
Common Psychological Triggers
Anxiety and panic disorders.
Depression.
Post-Traumatic Stress Disorder (PTSD).
Psychosomatic disorders, where mental stress manifests as physical symptoms.
The Burden of Psychological Chest Pain in Africa
a. Prevalence
While comprehensive data on psychological chest pain in Africa is limited, studies suggest a significant burden, particularly in urban areas where socio-economic stressors are high.
b. Impact of Social and Economic Stressors
Poverty and Unemployment: Persistent financial strain is a common cause of chronic stress.
Conflict and Violence: Individuals in conflict-affected areas are more prone to PTSD and related chest pain.
Stigma and Discrimination: Mental health stigma leads to underreporting and untreated psychological conditions.
c. Link to Urbanization
Rapid urbanization has increased exposure to stressors like overcrowding, pollution, and work-related pressures, contributing to a rise in stress-related chest pain.
Causes of Psychological Chest Pain
a. Anxiety Disorders
Description: Excessive worry and fear trigger physical symptoms, including chest pain.
Mechanism: Hyperventilation and muscle tension during anxiety episodes mimic cardiac symptoms.
b. Panic Attacks
Symptoms: Intense chest pain, palpitations, shortness of breath, and a sense of impending doom.
Prevalence: Often mistaken for heart attacks, leading to unnecessary cardiac investigations.
c. Depression
Symptoms: Persistent chest discomfort due to a heightened perception of bodily sensations.
Mechanism: Altered pain perception caused by neurotransmitter imbalances.
d. Post-Traumatic Stress Disorder (PTSD)
Triggers: Traumatic experiences such as conflict, displacement, or violence.
Symptoms: Recurrent episodes of chest pain during flashbacks or anxiety-provoking situations.
e. Somatic Symptom Disorder
Description: Chronic focus on physical symptoms, such as chest pain, without an underlying medical cause.
Mechanism: Psychological distress amplifies the perception of minor physical sensations.
Diagnostic Challenges in Africa
a. Overlap with Physical Causes
Psychological chest pain often mimics cardiac or respiratory conditions, leading to extensive, unnecessary testing.
Misdiagnosis is common due to the high prevalence of infectious and non-communicable diseases in Africa.
b. Limited Mental Health Awareness
Mental health conditions are stigmatized, causing patients to seek help only for physical symptoms.
Healthcare providers may lack training to recognize psychological causes of chest pain.
c. Inadequate Resources
Limited access to mental health professionals and diagnostic tools in rural and underserved areas.
Few facilities offer psychological evaluation or therapy as part of routine care.
Management of Psychological Chest Pain
a. General Management Principles
Focus on addressing the underlying psychological condition rather than solely treating the chest pain.
Educate patients about the connection between mental health and physical symptoms.
b. Non-Pharmacological Approaches
- Psychotherapy
Cognitive Behavioral Therapy (CBT): Helps patients reframe negative thoughts and manage stress effectively.
Trauma-Focused Therapy: Useful for individuals with PTSD or past traumatic experiences.
- Stress Management Techniques
Breathing exercises, mindfulness, and relaxation techniques.
Community-based support groups for stress reduction.
- Lifestyle Modifications
Regular physical activity to reduce anxiety and improve overall health.
Healthy diet and sleep hygiene to support mental well-being.
c. Pharmacological Approaches
- Antidepressants:
SSRIs (e.g., sertraline) for anxiety and depression-related chest pain.
Tricyclic antidepressants for somatic symptom disorders.
- Anxiolytics:
Short-term use of benzodiazepines for acute panic attacks.
- Pain Modulators:
Gabapentin or pregabalin for chronic somatic pain.
d. Community and Primary Care Integration
Train primary healthcare workers to identify and manage mild to moderate psychological conditions.
Increase accessibility to mental health services in rural areas.
Preventive Strategies
a. Mental Health Education
Raise awareness about the connection between stress and physical symptoms.
Encourage early intervention for mental health issues to prevent chronic conditions.
b. Reducing Socio-Economic Stressors
Address poverty, unemployment, and social inequalities to reduce population-level stress.
Provide psychosocial support for communities affected by conflict or displacement.
c. Strengthening Healthcare Systems
Integrate mental health services into primary care.
Increase the availability of mental health professionals and counseling services.
Psychological and stress-related chest pain is a significant but underappreciated issue in African populations. Socio-economic challenges, cultural stigma, and limited mental health resources contribute to underdiagnosis and inadequate management. Addressing this issue requires a multi-faceted approach, including community education, strengthening healthcare systems, and integrating mental health services into primary care. By improving access to mental health care and addressing underlying stressors, African communities can better manage and reduce the burden of psychological chest pain.
HIV/AIDS and Opportunistic Infections Causing Chest Pain in Africa
HIV/AIDS remains a major public health challenge in Africa, accounting for a significant global burden of the disease. Opportunistic infections (OIs) are common in individuals with HIV/AIDS due to compromised immunity, and many of these infections can cause chest pain. This guide explores the connection between HIV/AIDS and chest pain in Africa, focusing on opportunistic infections, their clinical manifestations, diagnostic challenges, and management strategies.
Overview of HIV/AIDS in Africa
a. HIV/AIDS Burden
Prevalence: Africa accounts for over 67% of the global HIV/AIDS cases. Sub-Saharan Africa is particularly affected.
Impact: Weakened immune systems make individuals susceptible to OIs, including those affecting the lungs, heart, and esophagus, which can cause chest pain.
b. Immune Suppression and Chest Pain
Chest pain in HIV-positive individuals often indicates advanced immunosuppression.
The severity and cause depend on the patient’s immune status, typically measured by CD4 cell counts.
Opportunistic Infections Associated with Chest Pain
Opportunistic infections in HIV/AIDS patients often involve the respiratory or gastrointestinal systems, directly or indirectly causing chest pain.
a. Tuberculosis (TB)
Description: TB is the leading cause of death among HIV-positive individuals in Africa.
Symptoms: Persistent chest pain, cough, fever, and weight loss.
Mechanism: Pulmonary TB leads to pleuritis or cavitary lesions causing chest pain.
Prevalence: High in regions with HIV and TB co-epidemics, particularly in sub-Saharan Africa.
b. Pneumocystis Pneumonia (PCP)
Description: Caused by Pneumocystis jirovecii, common in patients with CD4 counts <200 cells/μL.
Symptoms: Chest tightness, dyspnea, and dry cough.
Mechanism: Diffuse alveolar damage and reduced oxygen exchange cause discomfort.
c. Bacterial Pneumonia
Description: HIV-positive individuals are at higher risk for infections by Streptococcus pneumoniae and Haemophilus influenzae.
Symptoms: Sharp pleuritic chest pain, fever, and productive cough.
Risk: Higher among smokers and those with coexisting conditions like TB.
d. Esophageal Candidiasis
Description: A fungal infection causing esophagitis, common in advanced HIV.
Symptoms: Burning chest pain, painful swallowing, and regurgitation.
Prevalence: High in individuals with low CD4 counts.
e. Cryptococcal Infections
Description: Cryptococcus neoformans can cause pulmonary cryptococcosis or cryptococcal meningitis.
Symptoms: Chest pain, shortness of breath, and fever in pulmonary cases.
f. Cytomegalovirus (CMV) Infection
Description: CMV can cause esophagitis or interstitial pneumonitis.
Symptoms: Severe retrosternal pain and respiratory discomfort.
Prevalence: Common in severely immunosuppressed individuals.
g. Kaposi’s Sarcoma (KS)
Description: An AIDS-defining cancer caused by Human Herpesvirus 8.
Symptoms: Chest pain due to lung involvement or pleural effusion.
h. Fungal Infections
Examples: Histoplasmosis and aspergillosis.
Symptoms: Chronic chest pain, fever, and cough.
Prevalence: Associated with endemic areas and poor environmental sanitation.
Diagnostic Challenges in Africa
a. Overlapping Symptoms
Many OIs present with similar symptoms such as fever, cough, and weight loss, complicating diagnosis.
b. Limited Diagnostic Resources
Scarcity of advanced diagnostic tools like CT scans, PCR, or bronchoscopy in rural areas.
Reliance on clinical symptoms and basic diagnostic tests, which may delay accurate diagnosis.
c. High Co-Infection Rates
HIV-positive patients are often co-infected with TB or other respiratory infections, masking the primary cause of chest pain.
d. Stigma and Healthcare Access
Fear of discrimination leads to late presentation, especially in rural areas.
Management of Opportunistic Infections Causing Chest Pain
a. General Principles
Prompt diagnosis and treatment are critical to prevent complications and reduce mortality.
Address the underlying infection and improve immune function with antiretroviral therapy (ART).
b. Specific Treatment Approaches
- Tuberculosis
Standard anti-TB therapy (e.g., rifampicin, isoniazid, pyrazinamide, ethambutol).
Concurrent ART initiation for HIV co-infection.
- Pneumocystis Pneumonia (PCP)
High-dose trimethoprim-sulfamethoxazole (TMP-SMX).
Corticosteroids for moderate to severe cases to reduce inflammation.
- Bacterial Pneumonia
Empirical antibiotic therapy targeting common pathogens.
Vaccination against pneumococcal and influenza infections.
- Esophageal Candidiasis
Fluconazole or itraconazole for fungal eradication.
- Cryptococcosis
Amphotericin B and fluconazole for pulmonary or systemic involvement.
- Kaposi’s Sarcoma
Chemotherapy, ART, and palliative care for symptomatic relief.
- Cytomegalovirus Infection
Ganciclovir or valganciclovir for systemic or esophageal involvement.
Prevention Strategies
a. Antiretroviral Therapy (ART)
Early initiation of ART reduces viral load, preserves immune function, and prevents OIs.
b. Prophylaxis for Opportunistic Infections
TMP-SMX for PCP prevention in individuals with low CD4 counts.
Isoniazid Preventive Therapy (IPT) for TB prevention in high-risk individuals.
c. Vaccination
Routine immunization against pneumococcal and influenza infections.
d. Nutritional Support
Adequate nutrition to improve immunity and general health.
e. Public Health Interventions
Expanding access to HIV testing and ART services.
Strengthening TB control programs in HIV-endemic areas.
Role of Healthcare Systems and Community Support
a. Strengthening Healthcare Infrastructure
Establishing diagnostic facilities and training healthcare workers in HIV/OI management.
b. Community Education
Awareness campaigns to reduce stigma and encourage early healthcare seeking.
c. Integrating Care Services
HIV/AIDS, TB, and respiratory care should be integrated to streamline diagnosis and treatment.
Chest pain in HIV/AIDS patients in Africa is often linked to opportunistic infections that thrive in the context of weakened immunity. Tuberculosis, PCP, bacterial pneumonias, fungal infections, and esophageal candidiasis are among the leading causes. Addressing this issue requires a multifaceted approach, including early HIV diagnosis, ART initiation, effective OI management, and strengthening healthcare systems. By reducing the burden of OIs, improving diagnostic capacity, and expanding community-based support, Africa can significantly mitigate the impact of chest pain among HIV-positive individuals.
The Link Between Sickle Cell Disease and Chest Pain in Africa
Introduction
Sickle Cell Disease (SCD) is a genetic blood disorder primarily affecting individuals of African descent. It is characterized by the production of abnormal hemoglobin, known as hemoglobin S, which causes red blood cells to assume a sickle shape. These abnormally shaped cells can obstruct blood flow, leading to various complications, including chest pain. In Africa, where SCD is most prevalent, chest pain remains a significant concern due to limited access to healthcare and the unique challenges posed by the disease in this context.
Understanding Sickle Cell Disease
Sickle Cell Disease is inherited when a person receives two copies of the sickle cell gene (one from each parent). Its hallmark symptoms include:
Chronic anemia due to the destruction of sickled red blood cells.
Episodes of pain (vaso-occlusive crises) caused by blocked blood vessels.
Increased susceptibility to infections due to spleen dysfunction.
Complications in various organs due to restricted blood flow and oxygen supply.
Chest Pain in Sickle Cell Disease
Chest pain in individuals with SCD can arise from several underlying mechanisms, with the most common being:
- Acute Chest Syndrome (ACS):
ACS is a severe complication of SCD characterized by chest pain, fever, coughing, and difficulty breathing.
It occurs due to sickled cells blocking blood flow in the lungs, leading to inflammation, infection, or fat embolism.
ACS is the leading cause of hospitalization and death in SCD patients.
- Vaso-Occlusive Crises (VOC):
During a VOC, sickled cells obstruct small blood vessels, causing ischemia and pain in the chest wall.
The pain can mimic other conditions such as pneumonia or myocardial infarction.
- Pulmonary Hypertension:
SCD can lead to elevated blood pressure in the lungs, resulting in chronic chest pain and shortness of breath.
- Infections:
Pneumonia and other respiratory infections are common in SCD patients and can manifest as chest pain.
- Musculoskeletal Pain:
Rib infarction or costochondritis (inflammation of the cartilage in the rib cage) may cause chest pain.
- Cardiac Issues:
Chronic anemia and vascular complications can lead to cardiac strain or heart failure, presenting as chest pain.
Challenges in Africa
- High Prevalence:
SCD affects up to 2% of births in Sub-Saharan Africa, with Nigeria alone accounting for over 50% of global cases.
- Limited Awareness:
Many communities lack awareness about SCD, leading to delayed diagnosis and mismanagement of symptoms like chest pain.
- Inadequate Healthcare Infrastructure:
Access to specialized care, diagnostic tools, and treatment options like transfusions or hydroxyurea is limited in many regions.
- Compounding Factors:
Malnutrition, malaria, and frequent infections exacerbate SCD complications, including those causing chest pain.
- Cultural and Socioeconomic Barriers:
Misconceptions about SCD and stigma discourage affected individuals from seeking timely medical care.
Management of Chest Pain in SCD
- Acute Care:
Hospitalization for oxygen therapy, pain management, and hydration is essential in severe cases.
Antibiotics or antivirals are administered in cases of infection.
- Preventative Strategies:
Regular use of medications like hydroxyurea to reduce the frequency of VOCs and ACS episodes.
Vaccinations and prophylactic antibiotics to prevent infections.
Blood transfusions for managing severe anemia or preventing complications like stroke.
- Supportive Care:
Adequate hydration, balanced nutrition, and pain management at home can reduce the risk of complications.
Psychosocial support to address the mental and emotional burden of living with SCD.
- Specialized Treatment:
Advanced interventions such as bone marrow transplantation, though not widely available, offer a potential cure for some patients.
Recommendations for Africa
- Improved Awareness:
Public health campaigns to educate communities about SCD, its symptoms, and management.
- Enhanced Healthcare Access:
Establishing dedicated SCD centers and training healthcare providers to manage complications like chest pain effectively.
- Affordable Treatment Options:
Subsidizing essential medications and therapies for economically disadvantaged families.
- Research and Advocacy:
Encouraging research on SCD in African populations to develop tailored solutions and advocating for government policies supporting affected individuals.
- Integration of Traditional and Modern Medicine:
Collaborating with traditional healers to integrate cultural practices with modern medical approaches.
Chest pain in Sickle Cell Disease is a multifaceted problem, especially in Africa, where the disease burden is highest. Addressing this issue requires a comprehensive approach encompassing education, improved healthcare access, and preventive strategies. With concerted efforts from governments, healthcare providers, and communities, it is possible to alleviate the burden of SCD and improve the quality of life for millions of affected individuals.
Public Health Strategies for Managing Chest Pain in Africa: A Comprehensive Guide
Introduction
Chest pain is a critical public health issue in Africa due to its diverse causes, ranging from cardiovascular diseases and respiratory infections to trauma and psychosocial stress. Effective management of chest pain is essential to reduce morbidity and mortality. However, the continent faces unique challenges, including limited healthcare infrastructure, socioeconomic disparities, and a high burden of communicable and non-communicable diseases. This guide outlines public health strategies for managing chest pain in Africa, with a focus on prevention, diagnosis, and treatment.
Understanding Chest Pain in Africa
Chest pain can be caused by various conditions, broadly classified as:
- Cardiovascular Causes:
Ischemic heart disease (e.g., myocardial infarction, angina).
Hypertension-related complications.
Pericarditis or myocarditis.
- Respiratory Causes:
Tuberculosis (TB), pneumonia, and acute respiratory infections.
Pulmonary embolism or pleural effusion.
Chronic obstructive pulmonary disease (COPD) and asthma.
- Gastrointestinal Causes:
Acid reflux (GERD) or peptic ulcer disease.
Esophageal spasms or rupture.
- Musculoskeletal Causes:
Rib fractures, costochondritis, or chest wall trauma.
- Psychological Causes:
Anxiety, panic attacks, and stress-related disorders.
- Rare or Regional Causes:
Sickle Cell Disease (SCD)-related acute chest syndrome in regions with high SCD prevalence.
Challenges in Managing Chest Pain in Africa
- Delayed Diagnosis:
Limited access to diagnostic tools such as ECGs, X-rays, and laboratory tests.
Misdiagnosis due to overlapping symptoms of infectious and non-infectious diseases.
- High Disease Burden:
Coexistence of communicable (e.g., TB, HIV) and non-communicable diseases (e.g., hypertension, diabetes).
- Healthcare Infrastructure Gaps:
Shortage of healthcare facilities, trained personnel, and emergency services in rural and underserved areas.
- Cultural Beliefs and Stigma:
Hesitancy to seek care due to traditional beliefs or fear of financial costs.
- Economic Constraints:
Inability to afford healthcare services, especially in low-income households.
Public Health Strategies for Managing Chest Pain
To effectively manage chest pain in Africa, a multi-pronged approach is essential, focusing on prevention, early diagnosis, treatment, and long-term management.
- Prevention Strategies
Health Education Campaigns:
Increase awareness about risk factors for chest pain, such as smoking, hypertension, and obesity.
Promote healthy lifestyle choices, including regular physical activity and balanced diets.
Vaccination Programs:
Implement widespread vaccination against respiratory infections like pneumonia and influenza.
Screening and Early Detection:
Community-level screening for hypertension, diabetes, and tuberculosis.
Regular monitoring of individuals with high-risk profiles (e.g., smokers, elderly, and patients with chronic diseases).
Reduction of Risk Factors:
Anti-smoking initiatives and public policies to limit tobacco use.
Environmental policies to reduce exposure to air pollution, which exacerbates respiratory conditions.
- Diagnostic Strategies
Training Healthcare Workers:
Equip frontline healthcare providers with skills to identify life-threatening causes of chest pain (e.g., heart attack, pulmonary embolism).
Access to Diagnostic Tools:
Increase availability of ECG machines, portable ultrasound devices, and X-rays in primary and secondary healthcare centers.
Invest in laboratory infrastructure for testing cardiac enzymes, TB, and other relevant markers.
Telemedicine and Mobile Health (mHealth):
Use telemedicine platforms to connect rural clinics with specialists for real-time consultations and diagnosis.
Treatment Strategies
Development of Emergency Services:
Establish ambulance systems and trauma centers for rapid response to acute chest pain cases.
Train paramedics and first responders in basic life support (BLS) and advanced cardiovascular life support (ACLS).
Integrated Care Models:
Ensure availability of essential medications, such as nitroglycerin, antibiotics, and anticoagulants, at all levels of healthcare.
Implement protocols for managing common causes of chest pain, such as heart attacks and respiratory infections.
Referral Systems:
Strengthen referral pathways to ensure patients with complex cases can access tertiary care facilities.
Community-Based Interventions:
Utilize community health workers (CHWs) to monitor patients with chronic diseases and provide basic care at the community level.
Long-Term Management and Rehabilitation
Chronic Disease Management Programs:
Establish programs for conditions like hypertension, diabetes, and asthma to prevent recurrent chest pain episodes.
Provide ongoing care for post-TB lung disease and other complications.
Psychosocial Support:
Address mental health issues related to stress, anxiety, and chronic illness through counseling and support groups.
Rehabilitation Services:
Cardiac rehabilitation programs for patients recovering from heart attacks or cardiac surgery.
Pulmonary rehabilitation for individuals with chronic respiratory conditions.
Policy and Advocacy
Strengthening Health Systems:
Advocate for increased healthcare funding to expand infrastructure and human resources.
Develop national guidelines for chest pain management tailored to regional contexts.
Insurance and Financing Mechanisms:
Promote health insurance schemes to reduce out-of-pocket expenses for diagnostics and treatment.
Research and Data Collection:
Conduct epidemiological studies to understand the prevalence and causes of chest pain in different regions.
Use data to inform policy decisions and prioritize resource allocation.
Success Stories and Case Studies
Rwanda’s Universal Health Coverage:
Rwanda has implemented community-based health insurance schemes that improve access to diagnostics and treatment for conditions causing chest pain.
South Africa’s Anti-TB Programs:
Integration of TB screening and treatment with chest pain management has significantly reduced TB-related morbidity.
Chest pain is a complex public health issue in Africa, necessitating coordinated efforts at multiple levels. By implementing preventive measures, improving diagnostic capacity, and ensuring timely treatment, public health systems can reduce the burden of chest pain and associated complications. Collaboration between governments, healthcare providers, and communities is crucial to achieving sustainable outcomes and improving the quality of life for millions across the continent.
Conclusion on Chest Pain Causes
Chest pain is a common symptom that can result from various possible causes, ranging from mild to life-threatening. It is often associated with conditions like a heart attack, pulmonary embolism, or coronary artery disease, where a blood clot or restricted blood flow to the heart muscle can cause severe pain. However, non-cardiac issues such as gastroesophageal reflux disease, lung problems, or chest wall inflammation can also contribute to the discomfort.
Some symptoms, such as weakness, lightheadedness, and pain radiating to other areas, might indicate a serious heart problem or aortic aneurysm, particularly when involving the inner layers of the blood vessels. While a panic attack or high blood pressure may cause similar sensations, it is critical to differentiate these from life-threatening conditions. People experiencing persistent or severe chest pain, especially when accompanied by symptoms like shortness of breath or dizziness, should seek immediate medical help.
Timely medical advice and intervention are vital for diagnosing the cause of chest pain. Whether the issue lies with the lungs, the heart, or another system, emergency treatment in the emergency room may be necessary to prevent complications. For those with conditions such as aortic aneurysm, coronary artery disease, or pulmonary embolism, prompt medical attention can be life-saving. If you or someone you know experiences unexplained chest pain, it is always better to err on the side of caution and seek emergency medical help immediately.
Key Points on Chest Pain Causes
- Chest pain is a common symptom with various causes, including issues with the heart, lungs, gastrointestinal system, and chest wall.
- Common causes include gastroesophageal reflux disease (GERD), coronary artery disease, heart attack, and pulmonary embolism.
- Serious cardiac conditions such as aortic dissection, aortic aneurysm, and blockage in the coronary arteries can lead to life-threatening pain.
- Non-cardiac causes like panic attacks, physical activity-related strain, or inflammation in the chest wall can mimic heart-related conditions.
- Myocardial issues, such as insufficient blood flow to the heart muscle, often stem from heart disease and require urgent attention.
- Lungs-related conditions, including pulmonary embolism, can present with sharp chest pain and difficulty breathing.
- The most common reason for seeking the emergency department is uncertainty about the condition causing the symptoms.
- Many people with severe chest pain require evaluation in the emergency room to rule out life-threatening conditions.